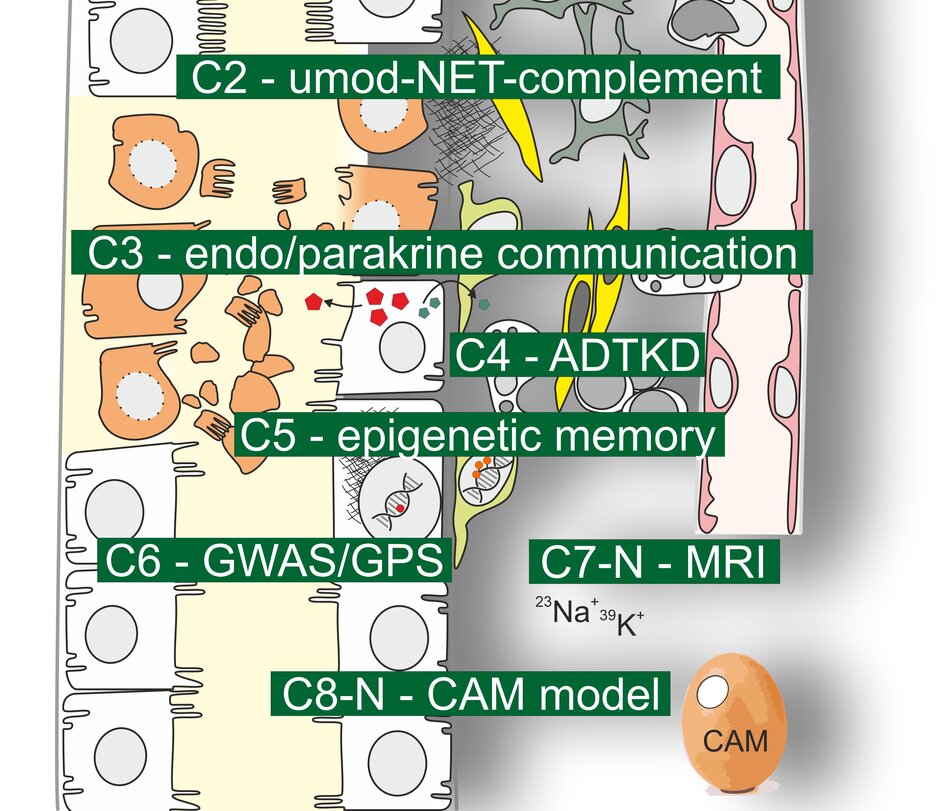
Crosstalk and (epi-)genetics
Research Area C includes projects on integrative topics of the tubulointerstitium with emphasis on interactions between different cell types and (epi-) genetics.
Project C2
Uromodulin-NET complement interaction in tubulointerstitial injury
Prof. Dr. Kerstin Amann (external link, opens in a new window), Nephropathology, University Hospital Erlangen
Prof. Dr. Maike Büttner-Herold (external link, opens in a new window), Nephropathology, University Hospital Erlangen
Prof. Dr. Dr. Christoph Daniel (external link, opens in a new window), Nephropathology, University Hospital Erlangen
This project aims to investigate the role and interaction of uromodulin (UMOD), neutrophil extracellular traps (NET) and the complement system in inflammatory and non-inflammatory tubulointerstitial kidney disease. To this end, we will investigate the presence, abundance and interaction of these three factors and their effects on inflammatory processes, fibrosis and renal function in human kidney biopsies, animal and in vitro models. Using inhibitor and knockout strategies, we will assess whether modulation of UMOD-NET-complement interaction could represent a new therapeutic target in tubulointerstitial kidney disease.
Project C3
Paracrine and endocrine communication in the renal tubulointerstitium
Prof. Dr. Frank Schweda (external link, opens in a new window), Physiology, University of Regensburg
Hormones, autacoids, and signaling metabolites are important determinants of intrarenal communication between different cell types and allow adaptation of one compartment to functional changes in another. Here, we will explore two pathways: i) the pathophysiological role of acetylcholinesterase in collecting ducts and ii) the relationship of interstitial renin and how tubular, interstitial, and juxtaglomerular renin interact in health and disease.
Project C4
Mechanisms of and interventional strategies against Autosomal Dominant Tubulointerstitial Kidney Diseases (ADTKD)
Prof. Dr. Michael Wiesener (external link, opens in a new window), Medical Clinic 4 - Nephrology and Hypertensiology, University Hospital Erlangen
The main objective of our project is to improve the molecular understanding of ADTKD, enabling us to design and validate interventional strategies in cellular and murine models. We aim to establish novel causative genes for ADTKD and thereby hope to gain more insights into disease mechanisms. Furthermore, we will generate and analyze patient-derived tubular cells by RNA-sequencing and metabolomics in order to identify novel pathway signatures. Finally, we will use patient-derived cells and murine models to validate interventional strategies (antisense oligonucleotides and BRD4780), principally suitable for clinical applications.
Project C5
The epigenetic memory of renal tubular cells
Dr. Steffen Grampp, Department of Medicine 4 - Nephrology and Hypertensiology, University Hospital Erlangen
Prof. Dr. Dr. Johannes Schödel (external link, opens in a new window), Department of Medicine 4 - Nephrology and Hypertensiology, University Hospital Erlangen
Epigenetic and transcriptional mechanisms in tubular cells governing acute kidney injuries and transition to chronic disease are only understood rudimentary, but may relate to important signaling pathways involved in promoting fibrosis such as hypoxia or inflammation. In order to analyze how hypoxia shapes an epigenetic memory in the tubular system, we will perform experiments in mice and isolated human primary cells using state-of-the-art genome-wide sequencing techniques. We will intersect this data with genetic predisposition studies to define mechanisms that might be susceptible to therapy in the future.
Project C6
Prioritizing genes for kidney function decline in the population and high risk groups
Prof. Dr. Iris Heid (external link, opens in a new window), Genetic Epidemiology, University of Regensburg
We will develop methodology for GWAS that is applicable for meta-analyses across numerous longitudinal GWAS. Based on our collaborations within the CKDGen Consortium, we will conduct such longitudinal GWAS for kidney function trajectories to identify and characterize genetic association loci for kidney function decline. We will also conduct genome-wide interaction studies to identify genetic effects on kidney function that are modulated by sex, age, diabetes status or obesity status. We will evaluate advanced methodological post-GWAS approaches for fine-mapping and annotation and develop an extended GenePrioritiSation (GPS-XL) for kidney function and kidney function decline integrating effective advanced methodology for post-GWAS, larger GWAS data, and genetic evidence across multiple kidney function biomarkers.
Project C7
Tissue distribution of K+ and Na+ in renal interstitial disease assessed by 39K and 23Na MRI
PD Dr. Christoph Kopp (external link, opens in a new window), Medical Clinic 4 - Nephrology and Hypertensiology, University Hospital Erlangen
Prof. Dr. Armin Nagel (external link, opens in a new window), Institute of Radiology, University Hospital Erlangen
In this project we will characterize the tissue electrolyte distribution in renal tubular dysfunction. We will therefore develop new MRI methodology to analyse tissue ion concentrations. Specifically, 23Na & 39K MRI will be applied to detect muscle Na+ & K+ shifts in aldosteronism. Furthermore, we will utilize combined morphological and 23Na imaging of the human kidneys to determine physiological Na+ variations. As tissue Na+ retention occurs in inflammation, we hypothesize that acute allograft rejection is characterized by tissue Na+ accumulation and can be detected by 23Na MRI. Besides, we will evaluate how SGLT-2 inhibitors influence the kidney Na+ and extrarenal Na+ & K+ concentrations in CKD and heart failure.
Project C8
3D in-ovo-model to study and modulate the growth of human renal cystic tissue and mouse kidney slices
Prof. Dr. Silke Härteis (external link, opens in a new window), Molecular and Cellular Anatomy, University of Regensburg
Prof. Dr. Thiha Aung (external link, opens in a new window), Applied Health Sciences, TH Deggendorf
Prof. Dr. Björn Buchholz (external link, opens in a new window), Physiology, University of Regensburg
The overall aim of our project is the translation of our findings of mechanisms of cyst growth resulting from animal models into clinical applications for the treatment of patients. We want to overcome this huge gap by introducing an intermediate model that allows us to monitor human cyst growth ex vivo and test promising drugs regarding their efficacy in human ADPKD tissue using the chorioallantoic membrane (CAM) model. Furthermore, the successful cultivation of vital adult mouse kidney tissue on the CAM may enable us to expand our studies to additional aspects of renal (patho-) physiology ex vivo.